


Sign-up for {N}power to get exclusive discounts, newsletters, members-only features, and more!
 Denver - Design District - Alameda and Broadway
Denver - Design District - Alameda and Broadway
368 S Broadway
Denver, CO 80209
United States
 Preferred Store:
Select a Store
Preferred Store:
Select a Store

For decades, dietary guidelines have generally suggested following a low-fat diet, however more recent well-designed studies are showing fat intake is beneficial for health. To add to this growing body of research, a 2021 peer-reviewed study in the journal Heart, Lung and Circulation found that dairy fat intake was associated with lower cardiovascular disease risk.1
 The researchers first measured the serum levels of pentadecanoic acid (a saturated fat known to be a biomarker for dairy fat consumption) in 4,150 Swedish 6o-year-old participants. The researchers followed the study participants for more than 16 years, collecting information about cardiovascular disease events and deaths during that time. After controlling for a variety of risk factors, the researchers found participants with the highest levels of the dairy fat biomarker pentadecanoic acid also had the lowest risk of cardiovascular disease.
The researchers first measured the serum levels of pentadecanoic acid (a saturated fat known to be a biomarker for dairy fat consumption) in 4,150 Swedish 6o-year-old participants. The researchers followed the study participants for more than 16 years, collecting information about cardiovascular disease events and deaths during that time. After controlling for a variety of risk factors, the researchers found participants with the highest levels of the dairy fat biomarker pentadecanoic acid also had the lowest risk of cardiovascular disease.
For the second part of the study, the researchers conducted a meta-analysis utilizing 18 different studies that looked at two dairy fat biomarkers (pentadecanoic acid and heptadecanoic acid) and cardiovascular disease risk. The results of the meta-analysis confirmed the results from the first part of the study, finding that higher levels of both dairy fat biomarkers were linked with lower cardiovascular disease risk.
This study differed from previous studies that compared high-fat and low-fat dairy from specific sources (e.g. milk, cheese, or yogurt). These previous studies raised doubts on the avoidance of dairy fat, leading to the thought that the benefits may be due to the type of dairy. However, the findings of the current study suggest high-fat dairy, regardless of the source, may be beneficial for supporting cardiovascular health.
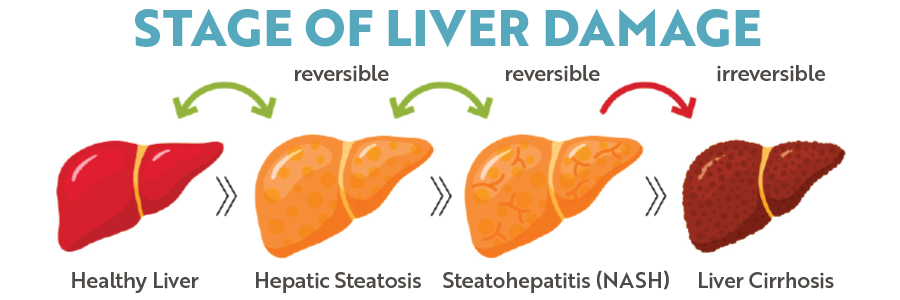
Brand new research2 shows that vitamin B12 and folic acid are inexpensive tools that could be used to prevent and/or delay the progression of an advanced form of Non-Alcoholic Fatty Liver Disease (NAFLD). NAFLD, classified as the buildup of fat in the liver, affects 25 percent of adults globally and is the leading cause of liver transplants. When NAFLD progresses to inflammation and scar tissue formation, it is known as non-alcoholic steatohepatitis (NASH). While fat deposition and NAFLD in the liver is reversible in its early stages, its progression to NASH is not and causes liver dysfunction, cirrhosis, and increases the risk of liver cancer.
Previous research has shown an association between NASH and high levels of homocysteine, an amino acid that vitamins B12, B6, and folate are required to break down; elevated levels increase the risk for serious health issues. As homocysteine levels increase in the liver, it can attach to various liver proteins, changing their structure and impairing their function. In particular, when homocysteine attaches to a protein called syntaxin 17, it blocks the protein from performing its role of transporting and digesting fat for metabolism, maintaining mitochondrial turnover, and preventing inflammation. This can lead to the development of fatty liver disease and NASH.
In the most recent study, published in July 2022, the researchers found that supplementing with vitamin B12 and folic acid increased the levels of syntaxin 17 in the liver and restored its role in its liver health-promoting mechanisms. It also slowed NASH progression and reversed liver inflammation and fibrosis.



Sign-up for {N}power to get exclusive discounts, newsletters, members-only features, and more!
